Toxic shock syndrome(TSS)
Toxic shock syndrome(TSS)
we hear horrifying stories about women who become gravely ill, lose limbs, or even die from toxic shock syndrome (TSS), a condition often associated with tampon use. If you’re someone who prefers tampons to other menstrual supplies, it’s easy to find yourself freaking out about whether you’re putting yourself in danger by using them. Take a deep breath – there’s no need to panic. There are a lot of myths about toxic shock syndrome out there, which make figuring out how to stay safe especially difficult. Lucky for you, this post is gonna set things straight.
TSS is a serious and dangerous condition, but you shouldn’t persistently worry about it, nor should you let the myths surrounding it prevent you from living the life you want to lead. By learning the facts about TSS – including how best to prevent it
Toxic shock syndrome is caused by the release of exotoxins from toxigenic strains of the bacteria Staphylococcus aureus and Streptococcus pyogenes in a person that lacks anti-toxin antibodies. These exotoxins act as superantigens.
In most cases, people with TSS will need to be hospitalized and closely monitored. When untreated, TSS can lead to shock, renal failure, and even death.
It’s also important to note that tampons aren’t the only objects associated with TSS – any device inserted into the vagina carries a risk. That includes contraceptive sponges and diaphragms, as well as menstrual cups.
Causes
An infection caused by strep or staph bacteria can lead to toxic shock syndrome. These bacteria are common and usually don’t cause problems. But in rare cases, the toxins enter the bloodstream and cause a severe immune reaction. This reaction causes the symptoms of TSS.
- Toxic shock syndrome caused by strep most often occurs after childbirth, the flu (influenza), chickenpox, surgery, minor skin cuts or wounds, or injuries that cause bruising but may not break the skin.
- Toxic shock syndrome caused by staph most often occurs after a tampon is kept in too long (menstrual TSS) or after surgery (non-menstrual TSS).
Risk factor
The following are risk factors for toxic syndrome:
- History of using super-absorbent tampons
- Surgical wounds
- A local infection in the skin or deep tissue
- History of using the diaphragm or contraceptive sponge
- History of recent childbirth, miscarriage, or abortion
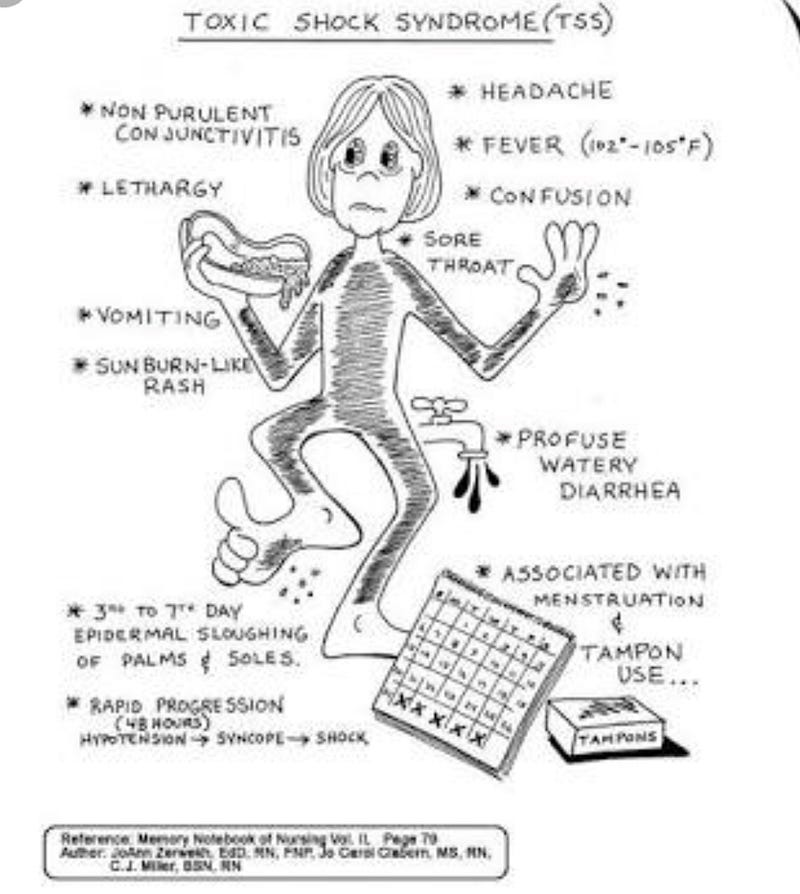
Symptoms
the following are the most common symptoms of Staphylococcal TSS:
- Fever higher than 102°F (38.9°C)
- Chills
- Feeling unwell
- Headache
- Fatigue
- Rash that is red and flat and that covers most of the areas of the body
- Shedding of the skin in large sheets, especially over the palms and soles, which is seen one to two weeks after the onset of symptoms.
- Low blood pressure
- Vomiting
- Diarrhea
- Muscle pain
- Increased blood flow to the mouth, eyes, and vagina, making them appear red
- Decreased urine output and sediment in urine
- Decreased liver function
- Bruising due to low blood platelet count
- Disorientation and confusion
TSS may start like other infections, but it can quickly progress to a seriously life-threatening disease. If a mild illness quickly becomes severe with whole-body symptoms, seek immediate medical attention.
Prevention
You can take following steps for prevention towards TSS :
- Keep all skin wounds clean to help prevent infection. This includes cuts, punctures, scrapes, burns, sores from shingles, insect or animal bites, and surgical wounds.
- Help keep children from scratching chickenpox sores by managing itching.
- Avoid using tampons and barrier contraceptives (such as diaphragms, cervical caps, or sponges) during the first 12 weeks after childbirth.
- If you have had menstrual TSS, do not use tampons, barrier contraceptives, or an intrauterine device (IUD).
Girls can reduce their risk of TSS by either avoiding tampons or alternating them with sanitary napkins. Girls who use only tampons should choose ones with the lowest absorbency that will handle menstrual flow, and change the tampons often. On low-flow days, girls should use pads instead of tampons.
Complications
Toxic shock syndrome is a life-threatening medical condition. In some instances, toxic shock syndrome can affect major organs in the body. If left untreated, complications associated with this disease include:
- liver failure
- kidney failure
- heart failure
- shock, or reduced blood flow through the body
Diagnosis
Your doctor may make a diagnosis of toxic shock syndrome based on a physical examination and your symptoms. Additionally, your doctor may check your blood and urine for traces of Staphylococcus or Streptococcus bacteria.
Your doctor may also do a blood test to check your liver and kidney function. They may also take swabs of cells from your cervix, vagina, and throat. These samples are analyzed for the bacteria that cause toxic shock syndrome.
Treatment
Treatment for toxic shock syndrome almost always takes place in a hospital. Treatment includes:
- Removing the source of the infection or cleaning the wound.
- Treating complications, such as shock or liver, kidney, and lung failure.
- Using antibiotics and other medicines to fight the infection.
- Sometimes surgery is needed if TSS developed after surgery or if the infection is destroying the skin and soft tissue (necrotizing fasciitis).
After having TSS, you may get better in 1 to 2 weeks. But it will take longer if you had major complications.
TSS is a very rare illness. Although it can be fatal, if recognized and treated promptly it is usually curable.
Related topics Links :
https://medium.com/@sonal9896225664/first-tampon-in-your-safe-period-womens-health-eb1f685d4c50?source=linkShare-e8f12eb6a57f-1529688912
Comments
Post a Comment